When is targeted therapy used in NSCLC?
Targeted therapy
Targeted anti-cancer drugs take aim at changes in cancer cells that they need to be able to grow. Targeted drugs tend to harm fewer normal cells than chemotherapy (chemo). This means targeted drugs may work even when chemotherapy does not. Targeted drugs may also have fewer or different side effects.
The changes targeted by this class of drug are sometimes called driver mutations (Table 1). Driver mutations help the cancer grow. Drugs targeted to these changes slow or stop the cancer. Your doctor may use a targeted therapy alone or with other drugs. Most of their use is for advanced lung cancer.
Targeted Driver Mutations in Advanced NSCLC

Types of targeted drugs
Anti-VEGF (also called antiangiogenic or anti-angiogenesis drugs)
- Bevacizumab (Avastin®)
- Ramucirumab (Cyramza®)
Anti-KRAS
About 1 in 8 people (13%) with NSCLC have a specific change in the KRAS gene called a KRAS G12C mutation. There are two anti-KRAS drugs that target this mutation.
- Sotorasib (Lumakras®)
- Adagrasib (Krazati®)
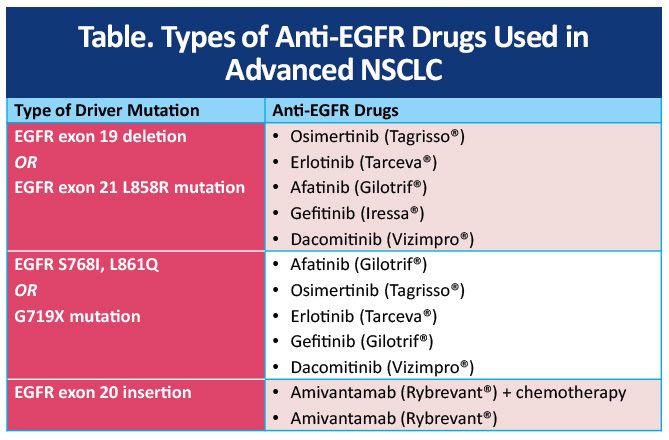
Anti-EGFR drugs
Several types of anti-EGFR drugs are used to treat NSCLC (Table 2). The targeted therapy used is based on the type of EGFR mutation in your cancer, and other things.
Drugs that target cells with ALK gene changes
About 5% of NSCLCs have changes in a gene called ALK. There are five anti-ALK drugs used to treat patients with advanced lung cancer that has an ALK alteration.
- Alectinib (Alecensa®)
- Brigatinib (Alunbrig®)
- Lorlatinib (Lorbrena®)
- Ceritinib (Zykadia®)
- Crizotinib (Xalkori®)
Drugs that target cells with ROS1 gene changes
About 1% to 2% of NSCLCs have a rearrangement in a gene called ROS1. Five oral drugs used to treat patients with advanced NSCLC that has a ROS1 alteration are:
- Ceritinib (Zykadia)
- Crizotinib (Xalkori®)
- Entrectinib (Rozlytrek®)
- Lorlatinib (Lorbrena®)
- Repotrectinib (Augtyro®)
Drugs that target cells with BRAF gene changes
Some NSCLCs have a specific change in a gene called BRAF (BRAF V600E mutation). Oral drugs used to treat NSCLC with this change are:
- Binimetinib (Mektovi®)
- Dabrafenib (Tafinlar®)
- Encorafenib (Braftovi®)
- Trametinib (Mekinist®)
- Vemurafenib (Zelboraf®)
Sometimes two of these drugs are used together, for example, dabrafenib with trametinib or encorafenib with binimetinib.
Drugs that target cells with RET gene changes
A small percentage of NSCLCs have changes in the RET gene. Oral drugs used most often to target advanced NSCLC with certain RET alterations are:
- Selpercatinib (Retevmo™)
- Pralsetinib (Gavreto®)
Drugs that target cells with MET gene changes
Some NSCLCs have a change in the MET gene called a MET exon 14 skipping mutation. Anit-MET drugs used to treat this type of change are:
- Capmatinib (Tabrecta®)
- Tepotinib (Tepmetko®)
On May 14, 2025, the US FDA approved elisotuzumab vedotin-tllv (Emrelis™) for use to treat certain types of locally advanced or metastatic NSCLC with high c-MET overexpression.
Drugs that target cells with HER2 gene changes
Some NSCLCs have a change in the HER2 gene that helps them grow. Trastuzumab deruxtecan or T-DXd (Enhertu®) is used to treat NSCLC with certain changes in HER2. Trastuzumab emtansine (Kadcyla®) is a less often used targeted drug.
Drugs that target cells with NTRK gene changes
A very small number of NSCLCs have changes an NTRK gene. Three drugs used to treat advanced NSCLC with certain NTRK gene changes are:
- Entrectinib (Rozlytrek®)
- Larotrectinib (Vitrakvi®)
- Repotrectinib (Augtyro™)
References
National Comprehensive Cancer Network
https://www.nccn.org/patients/guidelines/content/PDF/lung-metastatic-patient.pdf